Understanding Scalp and Hair Follicle Infections: Causes, Symptoms, and Treatments
Scalp and Hair Follicle Infections are common yet often misunderstood conditions that can affect anyone at any age. They not only pose aesthetic concerns but also cause discomfort and potential health complications. With the rise of various environmental factors and lifestyle choices, understanding these infections becomes paramount. This comprehensive exploration will cover the anatomy of the scalp, the diverse causes of infections, their symptoms, diagnosis, treatments, and preventive measures.
1. The Anatomy of the Scalp and Hair Follicles
Before we delve deeper into scalp and hair follicle infections, it is essential to understand the intricate structure of the scalp and hair follicles which serve as a foundation for comprehending how infections arise.
1.1. Structure of the Scalp
The scalp is composed of multiple layers of skin that protect the skull and house an intricate network of blood vessels, nerves, and hair follicles. This thin layer of skin has unique characteristics:
The outermost layer, or epidermis, serves as the first line of defense against external pathogens. Healthy epidermis plays an important role in maintaining the integrity of our skin barrier.
Beneath the epidermis lies the dermis, which contains connective tissue, hair follicles, sebaceous glands, and sweat glands. This rich supply of nutrients and moisture contributes to overall scalp health.
The vascular system within the scalp supplies oxygen and essential nutrients to the follicles, promoting healthy hair growth. The nerves present within this region relay signals related to touch, temperature, and pain, making the scalp sensitive to various external stimuli.
1.2. The Role of Hair Follicles
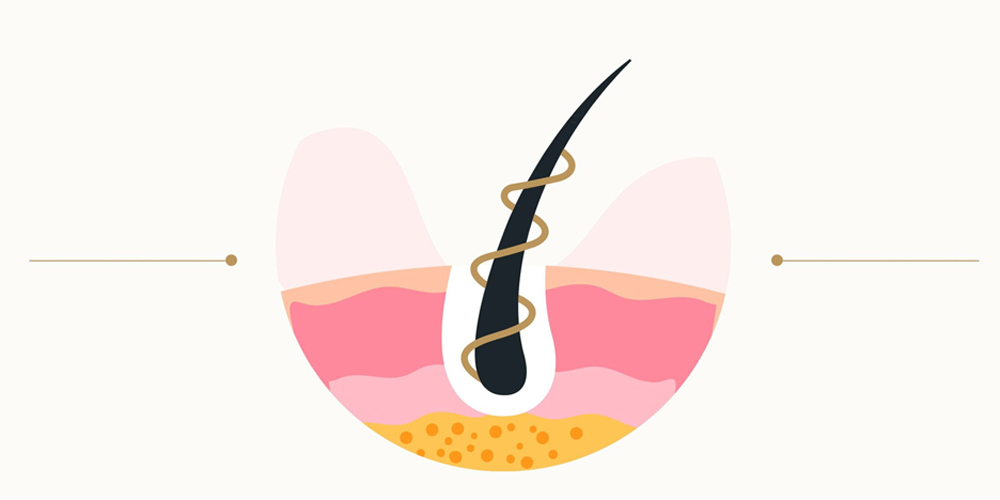
Hair follicles are dynamic organs responsible for producing hair strands. The anatomy of a hair follicle consists of several parts, including:
- Dermal Papilla: A small bulb-like structure at the bottom of the follicle that receives nutrients from blood vessels and stimulates hair growth.
- Sebaceous Gland: This gland produces sebum, an oily substance that lubricates the hair and skin, preventing dryness and maintaining pliability.
- Outer Root Sheath and Inner Root Sheath: These protective layers encompass the hair strand and play a pivotal role in shaping the hair’s texture and strength.
Understanding the structure and function of the scalp and hair follicles highlights their vulnerability to microbial invasion, setting the stage for infections to occur when conditions are favorable.
2. Causes of Scalp and Hair Follicle Infections
Scalp and hair follicle infections can be attributed to numerous factors ranging from fungal to bacterial and even viral origins. Each type of infection presents unique characteristics and symptoms that demand special attention.
2.1. Fungal Infections
Fungal infections are among the most common causes of scalp issues. One prominent example is Tinea Capitis, also known as ringworm.
This contagious infection primarily affects children and manifests through circular patches of hair loss accompanied by scaly, red skin. The fungi responsible thrive in warm, moist environments, making areas such as locker rooms or communal pools breeding grounds for infection.
An interesting aspect of Tinea Capitis is how it can lead to psychological distress in affected individuals, particularly children who may feel self-conscious about hair loss.
Another notable fungal culprit is Malassezia Globosa, a yeast that naturally resides on the scalp. An overgrowth of this fungus can result in dandruff or seborrheic dermatitis, characterized by greasy, flaky scales.
Understanding how these fungi interact with the scalp's natural flora emphasizes the need for maintaining a balanced environment to prevent infections.
2.2. Bacterial Infections
Bacterial infections, especially those caused by Staphylococcus aureus, frequently manifest as folliculitis. This condition entails inflammation of hair follicles, resulting in small, pus-filled bumps that can be itchy and painful.
While folliculitis may appear innocuous, it can evolve into more severe forms if left untreated, leading to significant health complications. Keeping one's scalp clean and free from excess oil can greatly reduce the risk of developing bacterial infections.
Cellulitis, another bacterial infection, affects deeper skin layers and displays alarming symptoms such as swollen lymph nodes and fever. This severe condition requires prompt medical attention to prevent systemic complications.
Impetigo, known to primarily affect children, can sometimes extend to the scalp. Its characteristic honey-colored crusts result from infected sores that require quick intervention to avoid spreading.

2.3. Viral Infections
Viral infections like the Herpes Simplex Virus (HSV) can wreak havoc on the scalp, causing painful blisters and sores. This virus is notorious for its recurrent nature, prompting outbreaks triggered by stress or illness.
Understanding HSV's link to scalp infections sheds light on the importance of managing stress and other predisposing factors.
Varicella-Zoster Virus (VZV), the same virus responsible for chickenpox, can lead to shingles-a painful rash that may affect the scalp.
Recognizing the potential consequences of viral infections encourages individuals to seek vaccination and awareness measures to mitigate risks.
2.4. Other Contributing Factors
While the aforementioned infections are primary causes, secondary factors can exacerbate susceptibility to scalp issues. A compromised immune system, whether due to conditions like HIV/AIDS or certain medications such as corticosteroids, increases vulnerability to infections.
Moreover, poor hygiene practices can lead to bacterial or fungal overgrowth. Regular cleansing and maintenance of scalp hygiene are vital to curtailing these infections.
Trauma to the scalp, stemming from burns or abrasions, can create entry points for pathogens, highlighting the dual role of protection and vulnerability inherent in scalp anatomy.
Awareness of these contributing factors accentuates the importance of preventive practices to maintain healthy scalps.
3. Symptoms of Scalp and Hair Follicle Infections
Identifying the symptoms of scalp and hair follicle infections is crucial for early diagnosis and treatment. Various infections manifest differently, but certain signs are commonly observed across different conditions.
3.1. Itching and Discomfort
Itching is one of the hallmark symptoms associated with scalp infections. Whether caused by fungal, bacterial, or viral origins, itching can range from mild to intense.
In fungal infections like Tinea Capitis, the pruritic sensation can lead to excessive scratching, further aggravating the affected area and increasing the risk of secondary bacterial infections.
Individuals experiencing persistent itching should consult healthcare professionals as it can indicate underlying infections requiring specialized care.
3.2. Redness and Inflammation
Inflammation and redness are critical indicators of infection. The affected area on the scalp might appear swollen and tender, signaling an immune response to the invading pathogens.
This response may be accompanied by heat, which serves as a physiological indicator of an ongoing inflammatory process. Understanding these symptoms empowers individuals to recognize when medical attention is warranted.
3.3. Scaliness and Flaking
Many scalp conditions, particularly those linked to fungal infections, exhibit excessive scaliness and flaking. Dandruff, often dismissed as a cosmetic issue, can disrupt daily life and negatively impact social interactions.
Seborrheic dermatitis takes it a step further, featuring greasy, yellowish scales alongside dryness. These visual symptoms not only highlight the presence of an infection but often have psychological ramifications for those affected.
3.4. Hair Loss and Pustules
Hair loss can occur due to severe infections like ringworm and folliculitis, where hair breaks off at the scalp level.
Pus-filled bumps associated with folliculitis signal an inflammatory response that can progress if untreated. The appearance of these pustules alerts individuals to potential bacterial infections needing immediate intervention.

3.5. Blisters and Systemic Symptoms
Viral infections can result in painful blisters that disrupt daily life, with accompanying systemic symptoms such as fever and chills.
These systemic manifestations are crucial warning signs indicating that the body is fighting an invasive pathogen, necessitating prompt medical evaluation.
4. Diagnosis of Scalp and Hair Follicle Infections
Diagnosing scalp and hair follicle infections requires a multifaceted approach involving clinical examination and testing methods. Accurate diagnosis is paramount to determining an effective treatment plan.
4.1. Physical Examination
A thorough physical examination allows healthcare professionals to visually assess the scalp and identify lesions, redness, scaling, or localized hair loss.
Through careful observation, practitioners can derive initial insights regarding the type of infection, guiding subsequent diagnostic steps.
4.2. Microscopic Examination
In many cases, scraping samples from the affected area undergoes microscopic examination to identify fungal spores or bacterial elements.
This process helps pinpoint the specific pathogen involved, allowing for a targeted approach to treatment.
4.3. Culture Tests
Culture tests involve taking samples of skin or hair and incubating them in laboratory settings to determine the predominant organisms.
By identifying the specific infectious agent, clinicians can prescribe the most appropriate antibiotic or antifungal medication, improving treatment efficacy.
4.4. Biopsy
Biopsies, although less common, may be necessary for more complicated cases. By extracting a small tissue sample, healthcare professionals can perform detailed analyses, enabling differentiation between various scalp conditions.
Understanding the intricacies of the diagnostic process empowers individuals to actively participate in their healthcare decisions.
5. Treatment of Scalp and Hair Follicle Infections
Once diagnosed, various treatment options are available tailored to the specific type of infection affecting the scalp and hair follicles. Treatment modalities range from topical medications to oral prescriptions, depending on the severity of the condition.
5.1. Antifungal Treatments
Fungal infections require specific interventions to eliminate the offending organism. Topical antifungal medications, such as ketoconazole or clotrimazole, are often the first-line treatments for mild cases.
These topical agents penetrate the scalp, targeting the fungal cells responsible for infections without causing systemic side effects.
In more serious scenarios, oral antifungal medications like terbinafine or itraconazole may be indicated.
These systemic therapies work from within, eradicating the infection effectively but may come with potential side effects warranting careful monitoring.
5.2. Antibacterial Treatments
For bacterial infections like folliculitis, topical antibiotics (e.g., mupirocin) can provide rapid relief by directly targeting the bacteria at the site of infection.
Oral antibiotics may be necessary in severe cases to ensure complete resolution and prevent complications such as cellulitis. Careful consideration of antibiotic sensitivity testing ensures effective treatment while mitigating antibiotic resistance.
5.3. Antiviral Treatments
Antiviral medications play a pivotal role in managing viral infections affecting the scalp. Acyclovir and valacyclovir are commonly prescribed for herpes simplex outbreaks, aiding in reducing the duration and severity of symptoms.
Prompt initiation of antiviral therapy can significantly lessen the impact of viral infections and promote quicker healing.
5.4. Other Treatments
In addition to the above, adjunctive treatments may include steroid creams to alleviate inflammation and itching. Warm compresses may also be beneficial, providing symptomatic relief by promoting circulation and promoting healing.
Education on proper scalp hygiene practices is vital. Encouraging individuals to wash their hair regularly and refrain from sharing personal items can help minimize the risk of reinfection or spreading infections to others.

6. Complications of Scalp and Hair Follicle Infections
When left untreated or inadequately managed, scalp and hair follicle infections can lead to various complications that may compromise both physical appearances and health.
6.1. Scarring and Permanent Hair Loss
Severe infections can result in permanent scarring on the scalp, ultimately leading to irreversible hair loss.
This outcome is particularly distressing, given the social implications associated with visible bald patches. Early intervention is essential to mitigate the risk of long-term damage.
6.2. Spread of Infection
Bacterial infections like cellulitis can spread rapidly beyond the scalp, impacting surrounding tissues and even entering the bloodstream.
Such dissemination could lead to systemic illnesses requiring hospitalization and intensive treatment, thereby heightening the seriousness of initially benign-looking infections.
6.3. Keloid Formation
In susceptible individuals, keloids—raised scars resulting from abnormal healing-can develop at the site of infection.
Keloids may become aesthetically displeasing and can also cause discomfort, prompting additional treatments for management.
6.4. Psychological Impacts
The psychological impact of scalp and hair follicle infections cannot be understated.
Individuals grappling with visible infections may experience anxiety and decreased self-esteem. Addressing the holistic aspects of treatment, including counseling or support groups, may offer valuable assistance.
7. Prevention of Scalp and Hair Follicle Infections
Preventing scalp and hair follicle infections is an achievable goal through diligent care and attention to hygiene.
7.1. Maintain Good Hygiene
Regularly washing the hair with gentle, non-irritating shampoos promotes a healthy scalp environment.
Avoiding harsh chemicals and products is crucial, as these can disrupt the scalp's natural flora and contribute to infections.
7.2. Avoid Sharing Personal Items
Sharing combs, brushes, hats, or towels with others poses a significant risk for transmitting infections.
Educating individuals on personal responsibility and hygiene practices is key to minimizing infection spread within communities.
7.3. Treat Existing Skin Conditions
Addressing underlying skin conditions like eczema promptly can prevent subsequent infections from developing.
Seeking dermatological guidance ensures that patients receive comprehensive care tailored to their unique needs.
7.4. Protection Against Trauma
Protecting the scalp from injuries, such as abrasions or burns, is vital.
Wearing appropriate hats or helmets in hazardous situations can reduce trauma and the associated risk of infections.
7.5. Strengthen Your Immune System
Maintaining a healthy lifestyle through balanced nutrition, regular exercise, and adequate sleep enhances immune function.
A robust immune system is better equipped to fend off infections and recover from potential exposures.
7.6. Follow Instructions for Medications
Proper adherence to prescribed medications is critical, especially for individuals on immunosuppressive therapies.
Being vigilant in following healthcare provider instructions enables better prevention of opportunistic infections.
Conclusion
Understanding scalp and hair follicle infections is crucial for effective management and prevention. The intricate anatomy of the scalp, coupled with knowledge of the various infections, symptoms, diagnosis, treatment, and preventive measures, empowers individuals to take charge of their scalp health. By understanding the root causes and recognizing the potential complications associated with these infections, individuals can make informed decisions about their health and well-being. Taking proactive steps towards maintaining good hygiene, seeking prompt medical attention when symptoms arise, and adopting a healthy lifestyle can drastically reduce the incidence and severity of scalp and hair follicle infections. Ultimately, fostering awareness around these conditions will not only benefit individual health but also contribute to the broader public understanding of scalp-related issues.
LATEST POSTS